R&D
A global pioneer in the development of new drugs
Research Areas
SK Biopharmaceuticals is pursuing the development of new, next-generation drugs with the goal of bringing safe and effective products to market to treat central nervous system (CNS) disorders. One of our core competencies is the ability to design drugs that can penetrate the blood-brain barrier*. Based on this capability, we have established a differentiated research pipeline for CNS disorders including both neurological and psychiatric disorders, and a chemical library of diverse compounds targeting CNS disorders. Also, we are focusing on the development of drugs for treatment of brain tumors. For this purpose, we are concentrating on the development of concurrently administered therapeutic drugs that can maximize the efficacy of targeted treatment drugs along with the treatment of the immune checkpoint inhibitor, utilizing a highly efficient screening (High Content Screening) system and cell strains and animal models in which the characteristics of patients have been reflected.
*Blood-brain barrier: the membrane that prevents penetration of specific substances from blood vessels into cerebral nerve tissues.
Epilepsy
What is epilepsy?
Epileptic seizure is the general term used to refer to abnormal symptoms in the sensory system, cognition, and behavior, caused by transient abnormal electric signals generated in the cerebral cortex.1 If these symptoms are accompanied by motor symptoms, they are referred to as convulsions.1 Epilepsy is a disorder in which recurrent convulsions or seizures occur without particular triggers such as electrolyte imbalance, acid-base imbalance, uremia, and alcohol withdrawal.1
Classification of epileptic seizures
The International League Against Epilepsy (ILAE) classifies epileptic seizures into two categories: partial onset seizures and generalized onset seizures.2
1) Generalized onset seizures
Generalized onset seizures refer to seizures that start from the broad area of both hemispheres of the cerebrum.1 There are various types of generalized onset seizures, including generalized tonic-clonic seizures, absence seizures, and atonic seizures.1
-
① Generalized tonic-clonic seizures
Individuals experiencing generalized tonic-clonic seizures display sudden unconsciousness from the initial stage of seizure, along with symptoms such as breathing difficulties, skin discoloration, and shouting, as well as a tonic phenomenon in which the entire body stiffens and the head turns to one side.1 After a period of tonicity (stiffening), the clonic (rhythmical jerking) behavior begins where arms and legs spasm due to repetitive tensing and relaxing.1,3 A deep sleep usually follows the seizure, and there is a possibility of a transient cognitive disorder as well as loss of memory for a period of time.1
-
② Absence seizures
Absence seizures occur mostly in young children.1 An affected child who has been displaying normal behavior will suddenly stop all activity without any warning, and will then blankly stare forward or upward for 5-10 seconds.1 Occasionally, the child may stare downward.1 This type of seizure may also be accompanied by a clonic seizure, with a slight fluttering of the eyelids or area around the mouth.1 Automatism behaviors, such as smacking of the lips or fidgeting with clothes, may also occur.1
-
③ Atonic seizures
In an atonic seizure, a person falls down due to a sudden loss of strength in the muscles of the entire body along with a sudden loss of consciousness.1 This is most often seen in Lennox-Gastaut syndrome, which manifests during early childhood and generally has a very poor prognosis.1
* Lennox-Gastaut syndrome is the severest form of epilepsy and manifests during early childhood between 1-8 years of age.4 It is a syndrome characterized by various types of convulsions, growth abnormalities, and behavioral disorders, such as impulse control disorder.4 This syndrome is known to have a poor long-term prognosis and is generally accompanied by a decline in cognitive function and sustained states of epilepsy (when epileptic seizure continues or consciousness is not recovered between seizures and unconsciousness occurs repetitively).4
2) Partial onset seizures
Partial onset seizures are caused by over-excitation of nerve cells and begin in one side of the cerebral cortex.1 There are various types of partial onset seizures, including simple partial seizures, complex partial seizures, and partial seizures with secondary generalization.1
-
① Simple partial seizures
These refer to situations in which the patient is awake and conscious when seizure occurs.1 The majority of simple partial seizures begin in one part of the cerebrum and do not spread to the entire cerebrum, so a state of consciousness is maintained.1 There are divers motor, sensory, and mental symptoms, depending on the area of the cerebrum affected.1 Motor symptoms include a flickering of one hand or arm or a droop on one side of the mouth1; sensory symptoms include abnormal sensations in the face, arm, or leg of one side of the body1; abnormal autonomic nervous system symptoms include a surging feeling, palpitations, goosebumps, or sweating1; and mental symptoms include recalling memories or experiencing familiarity of clearly unfamiliar objects or locations.1
-
② Complex partial seizures
Complex partial seizure is characterized by a disorder in the state of consciousness.1 Along with disturbances to consciousness d, recurrent behaviors, referred to as automatism, can occur.1 Frequently, behaviors such as smacking the lips together, fidgeting with nearby objects, or swinging hands aimlessly accompanied by a blank stare are observed.1 The individual generally does not remember that they are engaged in such a behavior.1 For seizures that occur in the non-dominant hemisphere of the brain, consciousness may be maintained, and the individual may speak and have a memory of what has happened, even with manifestation of automatism (although this is rare).1
-
③ Partial seizures with secondary generalization
This type is the most frequently observed form of epileptic seizure.1 Although symptoms of simple partial seizure or complex partial seizure are manifested in the initial stage of the seizure, it develops into a generalized onset seizure when the overactivity of the nerve cells proliferates to the entire cerebrum. The individual falls down and experiences a generalized tonic seizure, with their face turning blue in the initial stage.1 After a period of time, the seizure progresses to a shaking of the arms and legs.1
Causes of epilepsy
Epilepsy has no identifiable cause in about half the people with the condition. In the other half, the condition may be traced to various factors.5 It has been reported in an epidemiological study that more than one-third of individuals with epilepsy have a past history of brain disorders or brain damage, including strokes, encephalitis, and brain tumors.1 The causes of epileptic seizure can often be categorized according to age group.1
| Age | Causes of epileptic seizure |
|---|---|
| Birth-6 months | Damage in utero and following birth, abnormality in brain development, congenital malformation, acute infection of the central nervous system (CNS) |
| 6-24 months | Acute febrile convulsion, acute infection of the CNS, damage prior to and following birth, abnormality in brain development |
| 2-6 years | Acute infection of the CNS, damage prior to and following birth, abnormality in brain development, idiopathic (unknown cause), brain tumor |
| 6-16 years | Idiopathic, brain tumor, acute infection of the CNS, damage prior to and following birth, abnormality in brain development |
| Adult | Brain trauma, infection of central nervous system, brain tumor, cerebrovascular disease (stroke) |
(Ministry of Health & Welfare, Korean Academy of Medical Science)
Statistics
There are approximately 65 million individuals living with epilepsy worldwide, which is equivalent to 0.5-1% of the entire population.6 Epilepsy can impact people at any age, any gender, anywhere in the world.5 In particular, the prevalence of epilepsy is low in those below the age of 5, but then increases to about 6-8 persons per 1,000 people until the age of 10, and then remains at the same rate in accordance with the age bracket until it increases to affecting 14.8 persons per each 1,000 people for people over 75 years of age. This is closely related to the increase in the manifestation rate of epilepsy due to stroke or brain trauma during old age.1
Living with epilepsy
Individuals living with epilepsy may experience extensive difficulties due to seizures and the nature of the disease.1 They also suffer discrimination and restrictions due to stigma,7 and may face economic and psychological impacts during prolonged periods of illness.8 In addition, individuals living with epilepsy are at the risk for falling, drowning, or having a seizure while driving, along with experiencing depression, anxiety, or the risk of sudden unexpected death in epilepsy (SUDEP).9 Additionally, there are often other health complications to be addressed.9
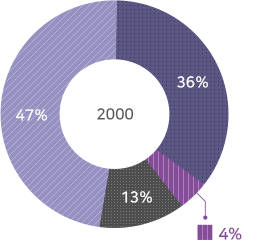
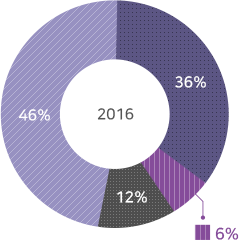
- Group reaching seizure-free state with primary drugs
- Group reaching seizure-free state with secondary drugs
- Group reaching seizure-free state with tertiary or multiple drugs
- Group failing to reach seizure-free state
- 1. Korea Centers for Disease Control and Prevention. National health information portal. Epilepsy (adult). http://health.cdc.go.kr/health/HealthInfoArea/HealthInfo/View.do?idx=6830
- 2. Berg AT, et al. Revised terminology and concepts for organization of seizures and epilepsies: Report of the ILAE Commission on Classification and Terminology, 2005–2009. Epilepsia, 51(4):676–685, 2010
- 3. Epilepsy Foundation. Tonic-clonic Seizures. Accessed on August 19, 2019. https://www.epilepsy.com/learn/types-seizures/tonic-clonic-seizures
- 4. Korea Centers for Disease Control and Prevention. Rare diseases. Lennox-Gastaut syndrome. http://helpline.nih.go.kr/cdchelp/ph/rdiz/selectRdizInfDetail.do?menu=A0100&rdizCd=RA201810560
- 5. Mayo Clinic. Epilepsy. Accessed on August 19, 2019. https://www.mayoclinic.org/diseases-conditions/epilepsy/symptoms-causes/syc-20350093
- 6. Epilepsy Foundation. Facts about Seizures and Epilepsy. Accessed on November 20, 2018. https://www.epilepsy.com/learn/about-epilepsy-basics/facts-about-seizures-and-epilepsy
- 7. World Health Organization. Epilepsy. Accessed on April 2, 2019. https://www.who.int/news-room/fact-sheets/detail/epilepsy
- 8. Allers K, et al. BMC Neurol. 2015; 15:245.
- 9. Epilepsy Foundation. Learn. Accessed on April 2, 2019. https://www.epilepsy.com/learn
- 10. Kwan P, Brodie MJ. N Engl J Med. 2000;342(5):314-319.
- 11. Chen Z, Brodie MJ, Liew D, Kwan P. JAMA Neurol. 2018;75(3):279-286.
Narcolepsy

What is narcolepsy?
Narcolepsy is a neurological disorder related to an abnormality in REM sleep, with excessive daytime sleepiness (EDS) as the main symptom.1 Other symptoms include cataplexy, in which the body is suddenly drained of energy during emotional stimulation, such as laughing loudly or getting mad, due to a disturbance in the sleep-wake cycle1; sleep paralysis, in which one is unable to move the body even though one is conscious at the time of falling asleep or waking up1; and hallucinations, in which dreams appear as reality at the time of falling asleep or waking up.1
EDS in narcolepsy
EDS refers to the onset of unbearable drowsiness even though one has had sufficient sleep during the night.1 People affected may fall asleep during classes or meetings, suddenly while speaking, and while driving, potentially causing traffic accidents.1
Prevalence
Narcolepsy is a disease with a worldwide prevalence rate of about 1 person for every 2,000 people,2 with the probability of children whose parents suffer from narcolepsy being affected by the disorder being about 1-2% percent.1 The disease occurs at a similar rate in males and females, with the highest incidence rate in people in their teens and 30s.1
Causes of narcolepsy
Narcolepsy is known to be associated with the human leukocyte antigen (HLA) found in the blood and a lowered concentration of hypocretin, which is a neurotransmitter involved in the control of the sleep-wake cycle.1 Narcolepsy occurs alongside a reduction of hypocretin nerve cells in the hypothalamus, a part of the brain that controls several important functions, including sleep.1
Sleep apnea
What is sleep apnea?
Sleep apnea is a sleep-related breathing disorder characterized by frequent waking during sleep due to reduced or stopped breathing when the upper airway narrows or gets blocked.3 Sleep apnea is defined as stopped breathing for more than 10 seconds during sleep.3 It can be classified into obstructive sleep apnea (OSA) if it occurs due to an obstruction of the airway in the oral cavity despite attempts to breathe, and central sleep apnea if breathing stops temporarily.3
EDS in obstructive sleep apnea
Daytime sleepiness and fatigue are the main daytime symptoms of sleep apnea sufferers3, with OSA known to be the greatest cause of EDS.4 Obstructive sleep apnea can affect concentration, decrease cognitive function, and impact individuals’ quality of life.5
Statistics
Sleep-related breathing disorders, in which apnea and hypopnea occur more than 5 times an hour, is observed in the United States in 24% of males and 15% of females 30-60 years old, with a prevalence of 4% of males and 2% of females experiencing sleep apnea accompanied by EDS.3 In Korea, sleep-related breathing disorders are observed in 27% of males and 16% of females 40-69 years old, with sleep apnea accompanied by EDS prevalence rates of approximately 4.5% in males and 3.2% in females.3
- 1. Korea Centers for Disease Control and Prevention. National health information portal. Narcolepsy. http://health.cdc.go.kr/health/HealthInfoArea/HealthInfo/View.do?idx=11600
- 2. Bhattarai J, Sumerall S. Sleep Sci. 2017 Jan-Mar; 10(1): 19–27.
- 3. Korea Centers for Disease Control and Prevention. National health information portal. Sleep apnea. http://health.cdc.go.kr/health/HealthInfoArea/HealthInfo/View.do?idx=3510
- 4. Ramar K, Guilleminault C. Sleep Med Clin. 2006;1:63-78.
- 5. Kapur VK, et al. J Clin Sleep Med. 2017;13(3):479-504.
Schizophrenia

What is schizophrenia?
Schizophrenia is a mental disorder that causes a broad range of abnormal clinical symptoms that affect cognition, emotion, perception, and behavior.1
Key symptoms of schizophrenia
1) Positive symptoms
Here the word "positive" means the presence (rather than absence) of symptoms.2 Positive symptoms include sensory abnormalities such as auditory or visual hallucinations, abnormal thoughts such as unrealistic and bizarre delusions, confused thoughts and disorganized speech.1,2
2) Negative symptoms
Negative symptoms refer to symptoms such as a reduction in normal emotional responses or behaviors, decreased ability to make decisions or to act, and social withdrawal.1 As a result of these symptoms, individuals with schizophrenia experience difficulties in conducting ordinary daily activities.1
3) Decrease in cognitive function
Decrease in cognitive function refers to difficulties in maintaining concentration and a reduction in the ability to learn new information or organize thoughts.1 As such, individuals with schizophrenia will not be able to perform tasks that they managed proficiently in the past, and they can experience a marked decrease in the ability to memorize information and the solve problems.1
4) Residual symptoms
Once schizophrenic patients overcome the severe acute stage, they enter the residual stage.1 During this period, the negative symptoms and cognitive disorders manifest as the main symptoms.1
Statistics
According to the World Health Organization (WHO), although schizophrenia affects more than 21 million people worldwide, its prevalence rate is not as high as many other mental disorders.3
Causes of schizophrenia
Based on current research, schizophrenia is known to be caused by a combination of genetic factors and environmental factors, rather than a single factor.1
1) Genetic factors
Schizophrenia is known to occur in families. While the probability of schizophrenia manifesting in people without family history is approximately 1%, the probability rises to about 10% for immediate family members of people with schizophrenia.1,4 Secondary immediate family members also display a higher manifestation rate of schizophrenia than people without a family history of schizophrenia.1
2) Biochemical/anatomical abnormalities in the brain
Neurotransmitters enable the cells in the brain to communicate and be linked with each other. It is known that there is an imbalance of neurotransmitters, including dopamine and serotonin, in people living with schizophrenia.1
In addition, the brains of people living with schizophrenia display minor differences when compared to the brains of healthy individuals, including a slightly larger cerebral ventricle containing cerebrospinal fluid, atrophy of gray matter, or a reduction in the metabolism of part of the brain.1 Brain cells of schizophrenic patients also display differences compared to those of healthy individuals.1 There is also a theory that, although these differences are determined before birth, they are not apparent during brain development, and once the brain changes at adolescence, such differences manifest and induce psychopathic symptoms.1
3) Environmental factors
Even if biological factors are the most fundamental cause of schizophrenia, psychological and environmental factors that individuals experience in utero and after birth, as well as during childhood, play an important role in the actual manifestation of schizophrenia.1
- 1. Korea Centers for Disease Control and Prevention. National health information portal. Schizophrenia. http://health.cdc.go.kr/health/HealthInfoArea/HealthInfo/View.do?idx=2400
- 2. WebMD. Schizophrenia Symptoms. Accessed on August 19, 2019. https://www.webmd.com/schizophrenia/schizophrenia-symptoms#1
- 3. WHO. Schizophrenia. Accessed on July 17, 2019. https://www.who.int/news-room/fact-sheets/detail/schizophrenia
- 4. WebMD. What Causes Schizophrenia? Accessed on August 19, 2019. https://www.webmd.com/schizophrenia/what-causes-schizophrenia#1
Attention Deficit Hyperactivity Disorder (ADHD)

What is Attention Deficit Hyperactivity Disorder (ADHD)?
ADHD is a mental disorder characterized by distraction, hyperactivity, and impulsiveness as the main symptoms.1 It mostly manifests in the early stages of childhood with a generally chronic progression.1
Statistics
According to a research conducted in the United States, approximately 2-6.3% of children in the United States are suffering from this disorder, while a prevalence rate of 2-4% has been reported in Korea.2 The disorder occurs 3-6 times more frequently in boys than girls.2
Causes of ADHD
The cause(s) and risk factors for ADHD are unknown, but current research shows that genetics plays an important role.3
1) Genetic factors
There are cases of children with ADHD that report a family history of the disorder; a study result shows that among children with ADHD, the manifestation rate in siblings is approximately 30% and, if the parents have ADHD, the manifestation rate in their children is 57%.1
2) Neurological factors
Failure to suppress behavioral responses occurs consistently, along with difficulties in performing other functions of the frontal lobe such as working memory, planning, linguistic fluency, and deciding motor sequence.1
3) Other risk factors
In addition to genetics, scientists are studying other possible causes and risk factors including exposure to environmental during pregnancy or at a young age; alcohol and tobacco use during pregnancy; premature delivery; and low birth weight.3
- 1. Korea Centers for Disease Control and Prevention. National health information portal. Attention deficit hyperactivity disorder. http://health.cdc.go.kr/health/HealthInfoArea/HealthInfo/View.do?idx=1540
- 2. Severance Hospital. Health column. Attention deficit hyperactivity disorder. https://terms.naver.com/entry.nhn?docId=2105411&cid=63166&categoryId=5102
- 3. Centers for Disease Control and Prevention. What is ADHD? Accessed on August 19, 2019. https://www.cdc.gov/ncbddd/adhd/facts.html
Bipolar Disorder

What is bipolar disorder?
Bipolar disorder is a treatable disease characterized by radical changes in mood, energy, thoughts, and behaviors.1 Such mood changes can last for several hours, weeks, or months.1 Bipolar disorder is also referred to as manic depression1
Classification of bipolar disorder
Bipolar disorder is classified into several types in accordance with the characteristics or severity of the symptoms. Bipolar I disorder and bipolar II disorders are most common.1
1) Bipolar I disorder
Bipolar I disorder is characterized by a manifestation of states of mania and severe depression.1 Generally, the number of depressive episodes is greater than the number of manic episodes.1 The duration that an individual displays normal moods in between the period of pathological mood states can vary.1
2) Bipolar II disorder
Bipolar II disorder is characterized by manifestation of states of mild mania and severe depression.1 This type is often erroneously diagnosed as unipolar depressive disorder.1
3) Unipolar depressive disorder
Unipolar depressive disorder is characterized by periods of severe depression.1 Although the extent of this type of depression ranges from mild to severe, it is not at the level of mania.1
4) Other types of disorders
There is a disorder called cyclothymic disorder (mania and depression that are not severe, which undergo cyclothymic occurrence for more than 2 years), and rapid cyclothymic type (more than 4 mood episodes of mania and depression occurring in a year).1 There is also unipolar manic state, which is the recurrence of mania with an otherwise normal mood.1
Statistics
Lifelong prevalence rates of bipolar I disorder and bipolar II disorder are approximately 0.4-1.6% and 0.5%, respectively.2 Rapid cyclothymic bipolar disorder, which presents as more than 4 episodes in a year, has a prevalence of about 15%.2
It is also known that approximately 1% of the entire population suffers bipolar disorder at least once in a lifetime.1 Although bipolar disorder frequently manifests as depression with the onset of the disease occurring most commonly at the end of adolescence, it can also manifest during childhood or in old age.1 There is almost no difference in the prevalence rates of bipolar disorder in males and females.1 However, males suffer mostly from a manic presentation and females from a depressive presentation.1
Causes of bipolar disorder
1) Chemical imbalance in the brain
Although the causes of bipolar disorder are not clearly understood, symptoms are known to occur due to chemical imbalance in the brain.3 The chemicals responsible for controlling the brain's functions are called neurotransmitters, and include noradrenaline, serotonin and dopamine. There's some evidence that if there's an imbalance in the levels of 1 or more neurotransmitters, a person may develop some symptoms of bipolar disorder.
2) Genetics
It is also thought bipolar disorder is linked to genetics, as it seems to run in families. The family members of a person with bipolar disorder have an increased risk of developing it themselves. But no single gene is responsible for bipolar disorder. Instead, a number of genetic and environmental factors are thought to act as triggers.
- 1. Korea Centers for Disease Control and Prevention. National health information portal. Bipolar disorder. http://health.cdc.go.kr/health/HealthInfoArea/HealthInfo/View.do?idx=1530
- 2. Severance Hospital. Health column. What is bipolar disorder? https://terms.naver.com/entry.nhn?docId=2105250&cid=63166&categoryId=51022
- 3. NHS. Bipolar disorder – Causes. Accessed on August 19, 2019. https://www.nhs.uk/conditions/bipolar-disorder/causes/
